Abstract
Introduction: The association between malignancies and venous thromboembolism (VTE) is a well established and significant cause of mortality in cancer patients. Compared to warfarin, low molecular weight heparin (LMWH) was found to be superior in preventing VTEs in the CLOT trial (Lee, et al. NEJM, 2003). Current guidelines recommend LMWH in patients with malignancies (Kearon, et al. Chest. 2016) however it is often difficult for patients to continue this long term given it is a subcutaneous injection that needs to be administered twice a day. Patients generally prefer direct oral anticoagulants (DOACs) due to ease of administration. When DOACs were compared to warfarin in non-cancer patients (RE-COVER, EINSTEIN, AMPLIFY, HOKUSAI-VTE trials), they had similar efficacy and safety profiles. There are limited studies looking at DOACs in malignancies, particularly in those with hematological malignancies who often present with cytopenias, making anticoagulation challenging. We performed a retrospective analysis to evaluate the efficacy and safety of DOACs compared to LMWH in patients with hematological malignancies.
Methods: We performed a retrospective analysis of patients diagnosed with a hematological malignancy who were placed on either a DOAC or LMWH for a VTE or atrial fibrillation (AF) from January 2011 to May 2017. We classified leukemia as those with AML, ALL, or CML and categorized CLL with other lymphoma subtypes. We also included multiple myeloma, MGUS, MDS, and Waldenstrom's macroglobulinemia. We primarily assessed efficacy and safety of DOACs in comparison to LMWH. Efficacy was based on incidence of a new VTE while on anticoagulation, and safety was measured by incidence of a bleeding event while on anticoagulation. CTCAE grading was used for bleeding events. 168 patients on DOACs and 70 patients on LMWH were available for analysis.
Results: Of the 168 patients on a DOAC, 108 (64%) were started for a VTE and 60 (36%) were started for AF. Of the 70 patients on LMWH, 67 (96%) were started for a VTE and 3 (4%) were started for AF. Median follow-up in the DOAC and LMWH group was 11 and 22 months, respectively. The groups were similar in median age, gender distribution, race, ethnicity, and malignancy types. Average weight between the DOAC and LMWH groups were 87 versus 90.5 kg, respectively. Estimated glomerular filtration rate was 81.2 mL/min/1.73m2 in the DOAC group and 86.6 mL/min/1.73m2 in the LMWH group. The majority of patients were diagnosed with either a lymphoma or leukemia (61.9% of patients with lymphoma/19.6% with a leukemia in the DOAC cohort, and 54.2% of patients with lymphoma/30% with leukemia in the LMWH cohort). The majority of patients had not yet achieved remission at time of DOAC/LMWH initiation (60.1% versus 58.6%, respectively). Apixaban was the most commonly prescribed DOAC (60.7%).
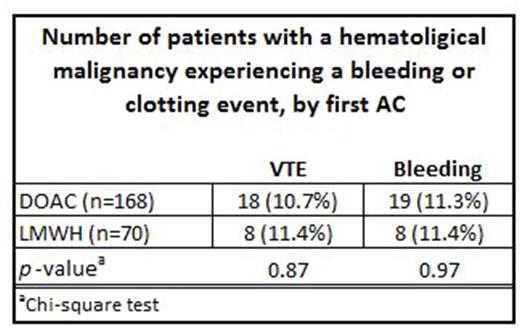
Incidence of a new VTE was 11.3% (n=18) in the DOAC group versus 11.4% (n=8) in the LMWH group. Of those who experienced a new VTE in the DOAC group, the majority developed a new extremity DVT (72.2%, n=13). Only two patients developed a new pulmonary embolism (PE), both of which were non-life-threatening. Of the 8 patients who developed a VTE in the LMWH group, 4 developed a recurrent extremity DVT (50%), 2 developed a thrombus in the IJ (25%), 1 developed a portal vein thrombus (12.5%), and 1 developed a submassive PE (12.5%).
The incidence of a bleeding complication on DOAC therapy was 10.7% (n=19) versus 11.4% (n=8) on LMWH therapy. Of the 19 bleeding events in the DOAC group, there were two intracranial bleeds, one grade 2 in the setting of a new stroke and the second considered Grade 4 after a mechanical fall. There were 6 gastrointestinal (GI) bleeding complications (3 grade 2, 3 grade 3). There were 3 grade 2 epistaxis and 3 grade 3 hemoptysis. There were two extremity hematomas and one abdominal hematoma after a trauma, all grade 3. Lastly, there were 2 grade 3 pericardial bleeding complications related to pacemaker exchanges.
Of the 8 bleeding events in the LMWH group, there was one grade 4 intracranial bleed after a new stroke and one grade 4 upper GI bleed in the setting of esophageal varices. Otherwise there were 4 extremity hematomas, (3 grade 2, 1 grade 3), one grade 3 leg hematoma and one grade 3 hemoptysis.
Conclusion: In those with hematological malignancies, DOACs appear to be non-inferior to the standard of care, LMWH, with similar efficacy and safety.
Portell: Infinity: Research Funding; TG-Therapeutics: Research Funding; Acerta: Research Funding; AbbVie: Research Funding; Roche/Genentech: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal